|
Eczema or atopic dermatitis is a chronic skin condition often causing red itchy inflamed skin which can range in severity from mild to severe. According to statistics around 15 million people in the UK live with this condition and in 2015 GP’s in England wrote around 27 million prescriptions for various topical agents costing around £169 million. If you are thinking to yourself that more and more people are suffering from this you’d be right in your assumption. An NHS funded study has shown that the numbers of cases have risen by 40 % in 4 years. What we do know about the condition is that it is an allergic condition with 80% of sufferers having raised IgE antibodies. Eczema patients have positive allergy tests and around two thirds have a family history. Many also suffer from other atopic conditions such as asthma and hay fever. The standard treatment protocols involve simply managing symptoms via emollients and sometimes steroids and if infection is triggered due to scratching, antibiotics. Allergens are also tested for although these tend to focus on only IgE mediated reactions. Other considerations…. Immune function We are back to finding our root cause. So first lets look at what’s going on in the immune system. The allergy antibody IgE is elevated in 80% of cases and this is activated by a type of white blood cell, a helper cell called TH2. Mast cells can release higher amounts of histamine leading to the itch that we associate with eczema. Then there’s the issue that around 90% of sufferers also have a predominance of the bacteria Staphylococcus aureus on the skin which their immune system is unable to kill. Often scratching can activate this infection and cause some potentially severe staph infections. So how do we prevent this vicious circle? Well we have to do everything we can from day one to promote our gut/immune function. In our immune system we have regularly T cells sometimes known as Treg, which are involved in immune suppression and immune tolerance. It’s known that an unhealthy gut can lead to a decrease in these important cells and therefore an imbalance in our TH1/TH2 cells with the TH2 cells being unregulated. Studies have indicated that the use of probiotics from birth can confer a reduction in TH2 dominance and symptoms of AD at 13 months old versus placebo. Breast feeding Studies have shown that breast feeding is associated with a reduced risk of eczema and other allergies. However there is a caveat here in that although breast milk may confer antibody protection, in at risk children it may also be necessary for the feeding mum herself to remove common allergens which may unwittingly be triggering the problem as these proteins pass through the milk. Common allergens being dairy, peanuts and eggs. That said, the advice is to introduce these common allergens while breast feeding at the 6 to 12 month stage and to then continue to breast feed for a further 6 months following this introduction. Older and formula fed children In older and formula fed children a study looking at triggers for eczema indicated that Peanuts eggs and milk have been shown to account for 80% of adverse reactions to foods in people living wth contact dermatitis. Other common triggers and are wheat, fish and soy. The hygiene hypothesis. Are we just too clean? Epidemiological studies, especially those looking at migration from one country to another indicate that we acquire the same immune disorders as soon as we move to another area so environmental factors are playing a huge role. Lifestyle changes have led to a decrease in infection in the industrialised world and this has been shown to be inversely correlated with increases in allergies and autoimmunity. Studies have also shown that exposure to animals or growing up on a farm confers protection from a young age as we are exposed to a greater variety of bacteria which leads to activation and modulation of innate and adaptive immune response. In one large Swiss study, nearly 14,000 children were surveyed between 2006 and 2007, with over 3,000 farming children and around 11,000 non-farming children. In this study, 38% of the non-farming children had allergies compared to 19% of the farming children. Digestive compromise Those living with allergies have commonly got some level of digestive compromise and dysfunction. Stomach acid which normally assists in the removal of infection and therefore has a protective role, can commonly become low and therefore play a role in weakening our immune system and make us more prone to infection. It also sets us up potentially for the leaky gut phenomenon which puts us at risk of further food sensitivities of the IgG variety (delayed reaction) and chronic inflammation. If you have intestinal permeability you may also be experiencing other health challenges e.g. fatigue, brain fog, headaches, depression, sinus, IBS, reflux, joint pain, and autoimmunity. This is also why I see many clients in clinic who may be coming along for help getting to the root of their eczema but who also have any number of the aforementioned symptoms. A lack of a very important nutrient zinc can ensue as a consequence of low stomach acid. This nutrient is essential for immune, gut, hormone and skin health. It affects appetite, smell and taste of food, so in children who have a narrowing of food choices and are no longer enjoying certain foods, zinc deficiency may be at the heart of this. It is also a particular problem in cases of acne in teenagers so look out for changes in eating and appetite in older children and test their zinc levels. This can be done with a very simple taste test which all the family can do. Adequate zinc is also required for healing the gut. Gut Flora and probiotics Because our immune system resides primarily in the gut we need to look at gut bacteria. We also need to weed out any trouble makers Interestingly yeast overgrowth is a common cause of eczema. It’s also a very common problem as the western diet of high sugar, refined carbs and low fibre sets up the perfect conditions for this to grow. In addition, yeast overgrowth can result from long term medication use e.g. antibiotics, steroids and the oral contraceptive pill. We therefore need to ‘weed and seed’ the gut, get the infections out and the good bacteria in to assist with immune balancing and symptom resolution. Risk factors for allergies in children This relates to those factors which influence the health of the micro biome from day one. In an ideal world we need to be focusing on the gut health of mum prior to a planned pregnancy as this is what baby inherits. Areas of concern are
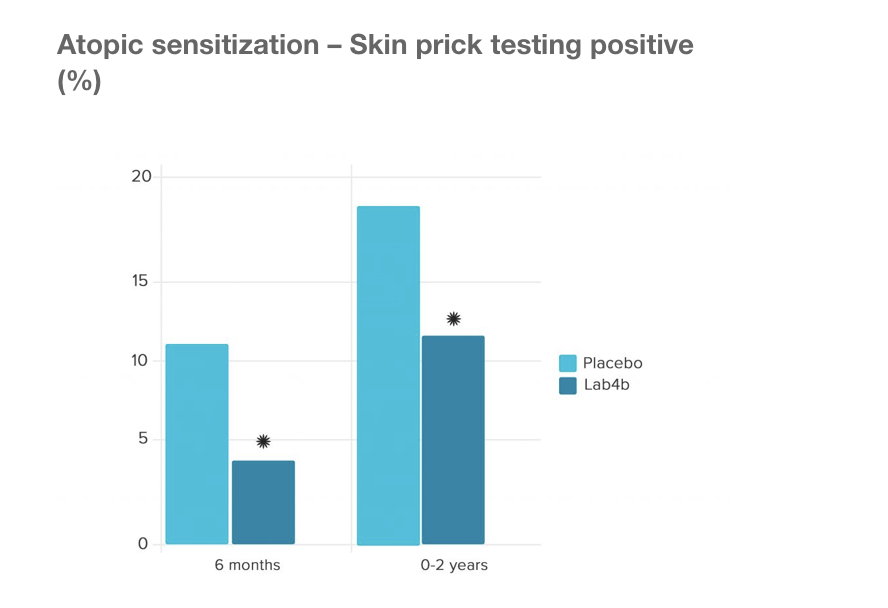
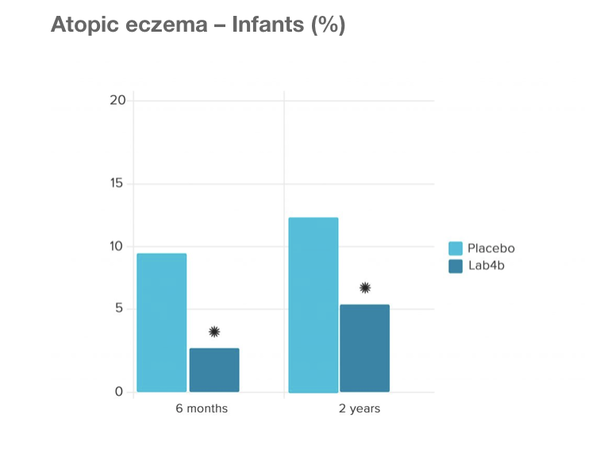
The Swansea Study This was a large study by the University of Swansea Medical School with 454 mother/baby pairs who were given Lab4b probiotics containing Lactobacilli and Bifidobacteria both during the final month of pregnancy and the first 6 months of infancy to evaluate whether this would prevent allergy in children. The results showed that versus placebo, the probiotic groups did indeed confer a protective effect on prevention of eczema and also prevention of allergic reaction to common allergens including pollen, cows milk, eggs and dust mites. Prof. Steve Allen, concluded the following key message from the trial:‘Lactobacilli and Bifidobacteria administered to pregnant women and infants aged 0-6 months prevented atopic sensitization and atopic eczema. The babies given the Lab4b probiotics were 57% less likely to develop atopic eczema than those receiving the placebo. The babies given Lab4b were 44% less likely to develop allergic reaction to common allergens, including pollen, cow’s milk, egg and house dust mite. Stress
Stress is very much linked with gut/immune function and when we are stressed we are more likely to have a flare of these conditions so managing stress for young and old is a life long strategy for eczema management. Adaptogen herbs can be helpful as can mindfulness, meditation and essential oils such as lavender for relaxation. As those living with eczema have a tendency towards poor absorption due to gut compromise a common nutrient which we can find ourselves low in is magnesium and this is also because we actually use more of it when we are stressed. More tips here on how to maintain levels. Nutritional therapy/ Functional medicine approach for eczema The nutritional therapy approach involved recognition of all of the above factors and follows through with the following stages.
Further testing This can be done if required and in addition to either allergy or food intolerance testing we can offer stool testing to identify infection and imbalance and even cortisol testing if stress is a particular trigger. Supplements This really does depend on the individual. It depends on what else they may be presenting with, their individual root cause/s, what medications they are on etc. However core supplements to include are going to be probiotics to reinoculate the gut, omega 3 and vitamin D. We may also recommend supplements and diet change to support gut integrity and immune balancing as per above recommendations. More info on booking an appointment with us for adults and children here. Referenced Studies Burks AW, Williams LW, Mallory SB, et al. Peanut protein as a major cause of adverse food reaction in patients with atopic dermatitis. Allergy Proceedings 1989;10:265-269. Von Mutius E, Vercelli D. Farm living: effects on childhood asthma and allergy. Nat Rev Immunol. 2010;10:861–868. Allen SJ et al 2014. Probiotics in the prevention of eczema: a randomised controlled trial. Archives of Disease in Childhood 99(11): 1014–1019
0 Comments
 Last year the Daily Mail published a fantastic story about a woman who managed to stop her migraines after cutting out corn and dairy products from her diet – with the help of a nutritionist and a food intolerance test! She had suffered terribly on a weekly basis for years on end, which is so sad to see when the cause was something as simple as eliminating a couple of foods from her diet. Food intolerance testing can help people tackle all sorts of conditions be it head related, stomach problems or skin conditions. I’m so glad I found out about it! I first developed eczema at the age of around 14 during my standard grade exams. The doctors put it down to stress, and not knowing any better, I simply agreed and went along with it. It was a pretty stressful time in my school life, and having never had any real problems with my skin prior to this, I guess it made sense at the time. Seven years later though, when the medicated creams failed to work time and time again, and the eczema kept coming back more and more aggravated each time, I began to question whether there could be something more to my flare ups than just stress. I visited Beverley in April last year for a food intolerance test – after my little brother had received his results for his own testing with regards to his abdominal pain. I was amazed that the test had managed to narrow down his problems to specific foods and as my brother had done so well and his symptoms had gone away I wanted to know if the foods I was eating on a day to day basis could be the culprit for my irritated skin! My results came back just one week later, and I took out chilli, garlic, ginger, yeast, gluten and dairy and was recommended to avoid these for 3 months and then re-introduce slowly and see how my skin reacted. It was definitely a thought to begin with – I was so used to eating whatever I wanted be it chocolate, crisps, pizza etc., I was a sucker for convenience food! I can honestly say now that my diet is much more varied and relatively healthy now which is a huge benefit having gone through this process. Since having switched my diet, I have seen a huge improvement in my overall health, not just my skin. My eczema has improved tremendously, and although it has flared up a little on my hands right now – this normally happens when the weather goes from one extreme to another. When my diet was mostly rubbish based, I would often take a nap during the day as I would get quite tired around 3pm. I can now function like a normal person from 6am – 11pm without a nap, which is a massive improvement as I can actually do things after work and with my evenings! Finally, the results that I have been most pleased with is my stomach. I no longer feel bloated on a day to day basis. I no longer need to eat and eat and eat to feel full, and I’ve lost around about a stone – solely from switching around my diet (and eating more!), and no extra exercise, which is amazing. I’ve since introduced all of the spices back into my diet with no problems as of yet – and I’m currently playing around with yeast too. At the moment I have no intentions of introducing dairy or gluten foods back into my diet. Of course this is all still a work in progress, however I’m absolutely delighted with all of my results. I feel a whole lot healthier on the inside and out - and would very much recommend a visit to a nutritionist if you feel that your diet could be improved, but you don’t know how to go about it. I also highly recommend Food Intolerance testing as it is life changing and saves years of unnecessary visits to the doctor and endless rounds of steroids. Wish I had done it sooner! - Lauren, Aberdeen If you would like to find out more about food intolerance testing or book an appointment pop in and see us at Nourishing Insights, 44 St Andrew Street, Aberdeen, AB25 1JA or call 01224 969637. Last week we covered Probiotics in Pregnancy and touched on how supplementing babies can help reduce the incidence of eczema and other allergies. But what about other common complaints in infancy? Can probiotics help there too? Let's look at some of the usual suspects: Colic is something that has troubled parents forever! The worst thing about colic is that we don't really know exactly what causes it. Having said that, anyone who has ever tried to comfort a colicy baby knows it's usually tummy trouble so trying a probiotic would make sense. A recent study now shows that introducing a probiotic has seen crying in infants fall by at least 50%. Another nightmare for new parents is reflux. (Not to be confused with 'happy pukers' it's totally normal for breastfed babies in particular to guzzle a little too much and then puke out the extra. It's part of their self regulation and why there is now a link between breastfeeding and reduced childhood obesity. If baby seems fine after they vomit you've probably got one of these!) Probiotics can be helpful here too. An Italian study has shown that probiotics can increase gastric emptying and therefore decrease the frequency of regurgitation. Constipation is also a common digestive problem in small children. Studies have shown that taking a probiotic can increase stool frequency and improve the consistency of stools. It has also been found to reduce the frequency of faecal incontinence and significantly reduce tummy pain. Severity and duration of boughts of diarrhoea have also been reduced by taking a probiotic. One finnish study found that the probiotics successfully colonized the gut and reduced the duration of watery diarrhoea usually associated with the rotavirus. In the ProChild study children were given either a placebo or Proven's Fit for School probiotic for six months. Children taking Fit for School had:
If you would like to know more or to discuss your probiotic needs with Beverley our registered Nutritional Therapist just pop into the shop: Nourishing Insights, 44 St Andrew Street, Aberdeen, AB25 1JA. References: A. Bird Schreck et al. (2016) Probiotics for the Treatment of Infantile Colic: A Systematic Review. Journal of Pharmacy Practice p1-9. F.Indrio et al. (2011) Lactobacillus reuteri accelerates gastric emptying and improves regurgitation in infants. European Journal of Clinical Investigation. 41(4) p 417-422. N. Bekkali et al. (2007) The role of a probiotics mixture in the treatment of childhood constipation: a pilot study. Nutrition Journal. 6(17) M. Tabbers et al. (2011) Is Bifidobacterium breve effective in the treatment of childhood constipation? Results from a pilot study. Nutrition Journal. 10(11) A.V. Shornikova et al (1997) Bacteriotherapy with Lactobacillus reuteri in rotavirus gastroenteritis. The Paediatric infectious disease Journal 16(12) p 1103-1107. I. Garaiova et al. (2015) Probiotics and vitamin C for the prevention of respiratory tract infections in children attending preschool: a randomised controlled pilot study. European Journal of Clinical Nutrition. 69 p.373-379. |
Amazon Associates DisclosureNourishing Insights is a participant in the Amazon EU Associates Programme, an affiliate advertising programme designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.co.uk. Archives
December 2023
|
WHAT OUR CLIENTS ARE SAYING“I did Nutritional Therapy with Beverley and it was life changing. I highly recommend it!” Allison Blakely (Glasgow)
|
Contact Us |