|
Vitamin D is one of the most common deficiencies. It is estimated that 1 billion people globally have Vitamin D deficiency and 50% of the global population have Vitamin D insufficiency. It is estimated that about 90% of our Vitamin D comes from exposure to sunlight whilst a small proportion comes from our diet. Individuals with darker skin have increased amounts of melanin in their skin which decreases the efficacy of Vitamin D absorption which is why people with darker skin are at greater risk, particularly in the UK where from October to March, the rays from the sun are not strong enough to enable our bodies to make vitamin D. This is one of the reasons that the Department of Health and the NHS now recommend that everyone in the UK should consider taking a vitamin D supplement from October to March. The elderly, overweight and those living in the Northern Hemisphere are also at greater risk. A 2017 study additionally revealed that shift workers, health care workers and indoor workers are at increased risk of developing a deficiency due to reduced outdoor time and sunlight exposure. Apart from this, malabsorption syndromes such as celiac disease, short bowel syndrome, gastric bypass and cystic fibrosis may also lead to Vitamin D deficiency. Medications such as phenobarbital, carbamazepine, dexamethasone, nifedipine, spironolactone, clotrimazole, and rifampin induce hepatic p450 enzymes which speed up the degradation of vitamin D.
Why do we need Vitamin D? Vitamin D's primary and vital function in the body is to maintain blood levels of calcium. It does this through increasing the amount of calcium absorbed from food in the small intestine. This helps the body to form and maintain healthy bones. A deficiency in vitamin D can lead to osteomalacia or rickets. A deficiency of vitamin D also increases the risk of developing osteoporosis and experiencing fractures and broken bones. Apart from this, vitamin D deficiency has also been associated with increased risks of cancer development, particularly breast, colon and prostate cancers. Researchers have found that increased sunlight exposure and circulating vitamin D are associated with reduced occurrence and mortality in many types of cancer. Vitamin D is well known for its impact on the immune system and studies suggest that inflammation is often at the root of many modern autoimmune diseases including multiple sclerosis, rheumatoid arthritis, digestive disorders and high blood pressure. University of Aberdeen researchers studied patients in the North of Scotland which has the highest rate of MS in the UK who were treated during the winter with UV-B light therapy. Dr Anthony Ormerod, Clinical Reader in Dermatology at the University, said: “Our study shows that UV-B light, which mimics sunshine, can have a striking effect on the immune system of patients." In addition, a study in 2018 from Trinity College Dublin linked vitamin D deficiency with an increased risk of depression of over 75% over a four year follow up period. What are the symptoms of Vitamin D deficiency? There is evidence to suggest that people with vitamin D deficiency are at increased risk of developing health conditions such as osteoporosis, autoimmune conditions, depression and cancer. Symptoms can also include weakness, chronic fatigue, depression, insomnia, anxiety, weakened immune system, inflammation and weak or broken bones. We would recommend that you are tested for vitamin D deficiency if you experience any of these symptoms. Vitamin D tests are available on the NHS and in our Nourishing Insights clinic. This is a simple pin prick blood test which can be done at home. Find out more about Vitamin D testing and order here. How can I optimise my vitamin D levels? The main way in which we obtain vitamin D is from exposure to natural sunlight from the sun. When UVB rays land on the skin, a substance in the skin, 7-dehydrocholestrol is converted into vitamin D3. There are two types of supplemental vitamin D; Vitamin D2 and Vitamin D3. The type of vitamin D our bodies makes naturally is vitamin D3. Whilst the body is able to convert some D2 for use, vitamin D3 is believed to convert 500 times faster than D2 and is estimated to be four times more effective in humans. Most experts suggest spending 20 minutes in the sun without suncream (suncream blocks the absorption of vitamin D) to enable your body to absorb vitamin D naturally without damaging the skin. For darker skinned people, the time recommended increases to around 40 minutes. If you do not want to expose your skin to the sun, you should use a good quality supplement to make sure you are obtaining enough vitamin D to protect your immune system, bones, joints and general health. Are there any food sources? Sunlight is the best source of vitamin D and it is difficult to obtain vitamin D only from food. However, there are some food sources and research suggests that eating foods which are rich in Vitamin D can help you acquire more. Some of the best sources of vitamin D in foods are halibut, mackerel, salmon, herring, trout and eggs. Mushrooms are one of the only plant sources of vitamin D and they acquire vitamin D the same way the human skin does, through exposure to the sun. The vitamin D content of mushrooms is increased through exposure to Ultra Violet light. The quantity of vitamin D in mushrooms can vary dependant on how they are grown. Who should supplement and how much should I take? Current Department of Health recommendations suggest the following ‘at risk’ groups should be using a vitamin D supplement all year round. These include:
From October to March the Department for Health recommends that everyone should supplement with Vitamin D. However, bare in mind that many of us now are spending little time in the sun and when we are we are wearing sun creams or covering up. Even in hot countries where people are going from air conditioned homes to offices and malls with little exposure to sunshine has led to a global epidemic with deficiency. For example, in countries such as Pakistan it is estimated that 80% of the population is deficient. In addition, it is estimated that vitamin D has a half life of about 15 days which would mean that every 2 weeks our levels halve without ongoing exposure to sunshine or supplementation. Therefore, your holiday in the sun in February is not going to help you in April. Dosages vary according to age, bodyweight and level of deficiency. Testing is recommended to optimise your dose. Are there other nutrient considerations when supplementing with Vitamin D? Vitamin D and K2 Vitamin D and Vitamin K2 work synergistically with each other to ensure that calcium is directed out of the arteries and into the bones where it helps improve bone density. Without enough vitamin K2 calcification within the arteries can occur. We normally advise a combination product of D and K2 for the post-menopausal age group. Vitamin D and Magnesium Magnesium plays a key role in determining how much vitamin D our bodies can make. It’s suggested that people whose magnesium intake is high are less likely to have a vitamin D insufficiency than people whose magnesium levels are low. It’s also claimed that magnesium supplementation increases vitamin D levels in people who are deficient in the vitamin, but causes a reduction in people whose intake is high. Too much vitamin D can increase calcium levels, which in turn can lead to certain health complications. To learn more about magnesium and signs of deficiency, have a look at our blog. To find out more about Vitamin D supplementation contact us here, or come and visit us at 44 St Andrew Street Aberdeen. Nutritional Therapy consultations are also available on Zoom and skype. More information here.
1 Comment
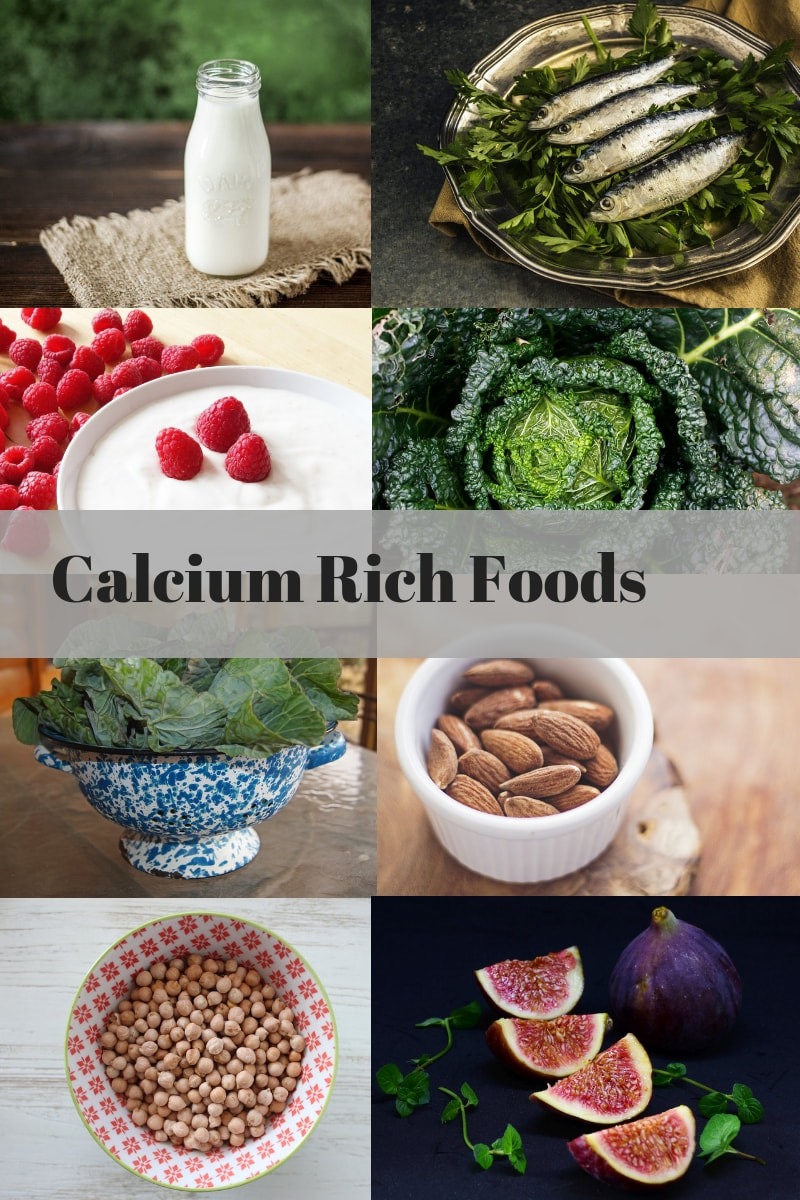
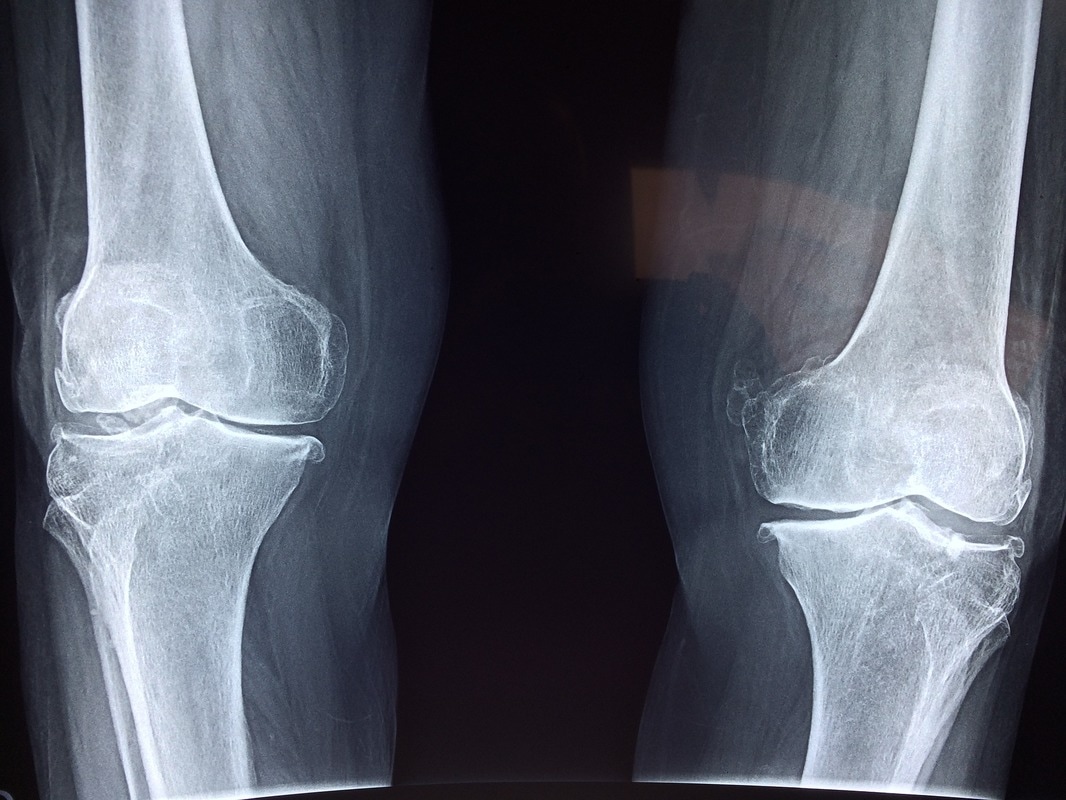
Calcium is an essential mineral for bone and teeth health. Although almost 99% of calcium is found in the bones and teeth, it is also found in the blood, muscles and other tissues. Calcium plays an important role in heart and nerve health, blood clotting, hormone secretion and muscle contraction. Additional functions include helping to control levels of magnesium, potassium and phosphorus in the blood. Calcium is the most abundant mineral in the human body, and so it is vital that we are meeting our requirements for optimal health. Calcium is clearly a vital mineral for health, but in order to maximise the benefit of consuming calcium rich foods, there are other factors we have to consider. For example, did you know that to properly absorb calcium, we also need magnesium, vitamin D and vitamin K2. If we don’t have adequate amounts of these vitamins on board, our ability to absorb any calcium we do eat is impaired. This is one of the reasons why it is better to get the calcium our bodies require from food sources or complex food supplements rather than isolated calcium supplements which aren’t always well absorbed. So what are the best food sources of calcium? Some of the best sources of calcium include sardines, organic milk, organic yoghurt and kefir, kale, collard greens, chickpeas, almonds and figs. Other good sources include sweet potatoes, bone broth, green leafy vegetables, beans, and broccoli. Currently, the NHS recommended daily allowance of calcium is 700mg, although you will see other experts recommending that we consume up to 1000mg per day for adults and 1200mg for over 50 year olds. However, the key thing we have to consider is absorption. As I always explain to people, we are not just what we eat, nor are we just what we absorb of what we eat, but we are also what our food ate! Impact of changing farming practices Intensive chemical farming practices have impacted minerals in the soil leading to our foods being depleted of vital minerals such as magnesium and calcium. Some conventional farmers have stopped properly rotating crops and replenishing the soil with natural fertilisers such as manure, which means our foods are much lower in calcium than they were in our grandparents time. Our advice therefore, is where possible to choose organic foods which have been shown to have higher nutrient value and higher antioxidant value in numerous studies, the largest to date being from Newcastle University. Other absorption challenges Gastrointestinal problems and conditions such as IBS, leaky gut syndrome, reflux, IBD and coeliac disease cause further problems with the absorption of nutrients. Any inflammation in the digestive tract impairs the absorption of nutrients. Counterintuitively therefore consuming dairy when you have a dairy intolerance does not mean that you will be able to absorb all the calcium from the food. Malabsorption of nutrients is of particular concern for those with IBD and coeliac disease who are at higher risk of other conditions such as osteopenia and osteoporosis as a result of their condition. For this reason, they are also often deplete in a wide range of nutrients, regardless of how good their diets are. Other issues such as low stomach acid which can be caused by stress, H-pylori, bacterial infections, antacid use, proton pump inhibitors and certain other medications can also lead to the malabsorption of calcium and other minerals. Add to this the fact that many drug medications actually deplete much needed minerals and vitamins and you can see where we can fall into difficulties. Sometimes therefore supplementation may be needed to normalise areas of concern such as stomach acid levels and digestive enzyme function. Low Vitamin D Many people have low vitamin D levels which impacts calcium absorption in the body. This is of particular concern for people who live in the northern hemisphere as during the winter (from October to March in the UK) sunlight doesn't contain enough UVB radiation for our skin to be able to make vitamin D. As sunlight is our bodies primary source of vitamin D, this is of major concern and is one of the reasons why the NHS now recommends everyone supplement with vitamin D over the winter months. During the summer, suncreams also block vitamin D absorption which means that if you are not having at least 20 minutes of unprotected sun exposure every day, you may be deficient in this vital nutrient. Good levels of vitamin D3 are essential for calcium intestinal absorption as vitamin D can increase calcium absorption in the intestinal tract by up to four times the normal rate. We normally recommend a vitamin D dose based on body weight. If you would like to test your vitamin D to optimise levels, we have testing services available at the Aberdeen clinic. Low Vitamin K2 As we know, D3 helps the body to absorb calcium, but vitamin K2 helps the body carry the calcium to your bones. This is important as calcium which is absorbed but not properly utilised in the body may be deposited into soft tissue causing cysts. Excess calcium in the blood stream can also be deposited in the kidneys where it may cause kidney stone formation. Vitamin K2 also ensures that the calcium is properly utilized and doesn't bind to oxidized LDL cholestrol, creating plaques which can cause blockages in the arteries. It can be so easy to fall into the trap of finding our favourite foods and forget about the variety of nutrients and minerals we get from a range of foods. Look at the list above and think about whether you are incorporating a good range of foods with calcium. If you are concerned that you may not be or think you would find it hard to incorporate enough into your diet on a regular basis, or have any of the gastrointestinal problems listed, it may be a good idea to find a good supplement form. Supplements we normally recommend are in combination form, alongside other essential nutrients for bone health. For people with gastrointestinal problems, we often recommend transdermal products which bypass the gut and are absorbed directly into the blood stream. BetterYou have designed a range of supplements for people with these kinds of issues. We particularly like their magnesium and calcium mineral lotion for bone health and their vitamin D and K2 spray. If you have any concerns, or queries about optimal dosages you can always come and see us and ask for advice at 44 St Andrew Street, Aberdeen. Over time our joints can wear out and many people experience stiffness and pain as they get older. The good news is that there are lots of things you can do to support yourself to reduce inflammation and support your natural healing processes. With optimal nutrition we can reduce inflammation, protect cartilage, and ensure adequate levels of nutrients are reaching our bones and surrounding ligaments. Reducing Inflammation This topic always reminds me of a physiotherapist who I trained with in Nutritional therapy. What made her train was that she realised that there was only so much she could do as a physio and that to really make impactful change with her patients she needed to address underlying inflammation. One of the most important things we can do to reduce inflammation is to consume good fats. This means increasing anti-inflammatory omega-3s and decreasing inflammatory omega-6s. Ideally, our diets should contain a 1:3 ratio of omega-3 to 6. However sadly most western diets contain far too much with a ratio of nearer 1:16 of omega-3 to 6. To reduce omega 6, avoid processed vegetable oils like sunflower and corn which are often found in processed foods. Great sources of omega 3 include oily fish e.g. salmon, mackerel and herring which we should try and eat at least twice a week. Wild fish contain a better ratio of fats so choose them over farmed where possible. Baking fish also helps to preserve the fatty acids much better than frying. Grass fed meat also contains omega 3s in the right ratio whilst grain fed meat should be avoided as it has much higher omega 6. Chia seeds, ground linseed, hemp seeds and walnuts are great plant based sources of omega 3 and can easily be added in to breakfast cereals or sprinkled over fruit and yoghurt. For those struggling to increase their intake, taking a high strength fish oil or flax seed oil can help reduce inflammation and severity of symptoms. Increasing Antioxidants A Finnish study has shown that low serum levels of antioxidants increases the risk of rheumatoid arthritis. A diet rich in antioxidants can help to reduce oxidative stress and inflammation often associated with arthritis and joint pain. The easiest way to up your antioxidants is to eat a rainbow of fruit and vegetables. Curcumin found in turmeric is an antioxidant which has found favour recently as it has anti-inflammatory properties which have been shown to have therapeutic potential for the treatment of crystal-induced arthritis or rheumatoid arthritis. Exercise Exercise has been shown to reduce pain and increase physical function in adults with Osteo-arthritis. Of course, this should be appropriate to your fitness level but gentle exercise such as walking and swimming are just as effective. Exercise combined with a supportive diet will help to reduce excess weight which will then help decrease long term stress on the joints. How can I protect my joints? Glucosamine plays a role in the building of tendons, cartilage and synovial fluid in our joints. Our bodies ability to produce glucosamine is reduced with age. Supplementing with glucosamine helps our bodies to repair cartilage which may otherwise be damaged in arthritic joints. Chondroitin is often taken alongside glucosamine as it has been shown to modify joint based pathologies. MSM has been shown to decrease joint inflammation, improves flexibility and restores collagen production. Research shows that many patients with arthritis, joint pain, stiffness, knee/back problems and a limited range of motion experience a reduction in symptoms and improved quality of life when taking an MSM supplement. Nutrients that can support joint health Vitamins that are key to ensuring our joints stay healthy are Vitamin D, Calcium, Magnesium and Zinc. Vitamin D is really important in joint and bone health. Unfortunately, in the UK many of us are deficient as we just don’t get enough sunshine. Only 10% of our vitamin D requirement comes from food so it’s really important to try and get 20 minutes of sunshine per day (without sun cream which blocks our ability to absorb vitamin D). The NHS now recommend that everyone should supplement with vitamin D as we simply don’t get enough. Low vitamin D levels have been shown to increase risk of progression of osteoarthritis. In addition to supporting bone health vitamin D also helps to support the immune system. Women post menopause may also wish to consider taking a vitamin D and K supplement This combination has been shown to support uptake of calcium from the blood to the bone significantly more than supplementing with just D on it’s own. Calcium and Magnesium Everyone knows that calcium is important for bone health. However, supplementation of calcium on it’s own has been shown to make no difference. It needs to be taken alongside magnesium as the two work together. Magnesium is involved in the structural building of bones as well as in the transportation of calcium across cell membranes. Rich food sources of calcium include dark green leafy vegetables, dairy, almonds and sardines. Magnesium-rich foods include dark green leafy vegetables, nuts, seeds, beans and lentils. A great combo product is Osteoguard which contains Calcium and magnesium along with Vitamin D and K. Zinc Zinc is vital to support tissue growth and repair. It also helps to support the immune system and can be found in seafood, meat, wheat germ, nuts and seeds. Reducing Pain Devils claw is a great pain reliever for those suffering osteoarthritis. Boswellia also reduces pain by inhibiting inflammatory mediators and improving blood supply to the joints. We often recommend a lovely product by Pukka which contains Turmeric, Boswellia, Ginger and Red ginseng – ideal for someone with arthritis. Ginger is a well-known anti-inflammatory which can be used in the culinary form and is often seen in combinations with many of the above in products aimed at reducing inflammation. Food Intolerances Unfortunately due to the long term use of NSAID’s (non steroidal anti-inflammatory drugs) such as ibuprofen and steroids for pain management, we can find ourselves with damaged gut flora. This begins to show itself as new digestive symptoms from bloating to IBS and as a result we may begin to feel we have some issues with foods that we didn’t have previously. This is where food intolerance testing and some gut healing work with a registered and clinically trained Nutritional Therapist can be invaluable. As you can see HERE , those with musculoskeletal problems experienced a 64% moderate to high benefit. We work with a range of inflammatory conditions including osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis. (See testimonial below) It’s a complex subject but as ever, come and chat to us and we will help you unravel some of the challenges you’ve been having with your joints. To book a discovery call to find out more book here and if you would like to book for Nutritional therapy you can find out more here Patterson E, Wall R, Fitzgerald GF, Ross RP, Stanton C. Health implications of high dietary omega-6 polyunsaturated fatty acids. J Nutr Metab, 2012, 539426. Simopoulos, A.P., 2002. The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomedicine & pharmacotherapy, 56(8), pp.365-379. Heliövaara, M., Knekt, P., Aho, K., Aaran, R.K., Alfthan, G. and Aromaa, A., 1994. Serum antioxidants and risk of rheumatoid arthritis. Annals of the rheumatic diseases, 53(1), pp.51-53. Jackson, J.K., Higo, T., Hunter, W.L. and Burt, H.M., 2006. The antioxidants curcumin and quercetin inhibit inflammatory processes associated with arthritis. Inflammation Research, 55(4), pp.168-175. Golightly, Y.M., Allen, K.D. and Caine, D.J., 2012. A comprehensive review of the effectiveness of different exercise programs for patients with osteoarthritis. The Physician and sportsmedicine, 40(4), pp.52-65. Reginster, J.Y., Neuprez, A., Lecart, M.P., Sarlet, N. and Bruyere, O., 2012. Role of glucosamine in the treatment for osteoarthritis. Rheumatology international, 32(10), pp.2959-2967. http://openheart.bmj.com/content/2/1/e000300 Bischoff-Ferrari HA, Zhang Y, Kiel DP and Felson DT (2005) Positive association between serum 25-hydroxyvitamin D level and bone density in osteoarthritis. Arthritis and Rheumatism, 53: 821–826. I reached out to Beverley interested to try another approach to managing my symptoms of ankylosing spondylitis. Did you know that magnesium is an essential mineral for cellular health and over 300 biochemical functions in the body? As a result, deficiencies of this vital nutrient can create all kinds of health problems. Health complaints which magnesium deficiencies are commonly associated with include hormonal imbalance, behavioural disorders, mood swings, insomnia, fibromyalgia, chronic fatigue, migraine headaches, and type 2 diabetes. It is now estimated that a staggering 80% of people are deficient in this vital nutrient. What has led to widespread magnesium deficiency? The main causes of magnesium deficiency are gastrointestinal and renal losses. However, you can also lose magnesium through excessive sweating, every day movement and stress. Even if you regularly consume vast quantities of magnesium rich foods such as spinach and swiss chard, you still may not be receiving the levels of magnesium required for optimal health. This is because soil depletion has lowered the amounts of magnesium present in crops and magnesium has been stripped from processed foods. In addition, the increasing consumption of antibiotics both for medical usage and in the food chain has stripped our guts of the good bacteria necessary for proper digestion and absorption of vitamins and minerals. As the number of people with digestive disorders such as leaky gut has risen, as well as autoimmune conditions such as coeliac disease which inhibits the absorption of nutrients, this also makes it harder for people to absorb vitamins and nutrients such as magnesium. It may therefore be easier for people with these kinds of digestive complaints to absorb vitamins and minerals transdermally through the skin rather than the gut. BetterYou have created a great range of high quality magnesium oil sprays and bath salts which are great for people with these kinds of issues. What are the benefits of supplementing with magnesium? From regulating the heartbeat rhythms to helping neurotransmitter functions, magnesium is a vital nutrient for human health. There are numerous studies which have pointed to the benefits of supplementing with magnesium in conditions such as migraine, type 2 diabetes, muscle aches, depression and more. For example, a study in the Expert Review of Neurotherapeutics found that taking 300 milligrams of magnesium twice a day reduced the frequency of migraine headaches. Whilst another study in MMW Fortschr Med has found that people under mental and physical stress can benefit from a daily intake of magnesium to prevent symptoms of deficiency such as anxiety, depression, restlessness and insomnia. Magnesium can also aid digestion, and relieve constipation as it relaxes the muscles in the digestive tract. How do I know if I am deficient? If you are experiencing symptoms such as muscle aches or spasms, poor digestion, anxiety, headaches, a twitchy eye or insomnia it may be a sign that your levels of this mineral are low. Of course there may be other reasons for this, which is why if you are really concerned it is always best to speak with a Nutritional Therapist who will be able to assess your case and perhaps make additional or more appropriate suggestions. Magnesium on its own is not always a miracle cure! Particularly if there are other gastrointestinal issues or food intolerances. Another sign that you are low might be if you regularly crave chocolate which contains magnesium. As it has become the typical punchline that women crave chocolate around menstruation, it has been suggested that this is because chocolate contains magnesium which alleviates some of the symptoms associated with PMS such as pain and mood swings. However, dark chocolate contains far more magnesium than milk chocolate, so if you are after some magnesium rich chocolate it would be a dark chocolate which contains at least 70% cocoa solid (and preferably raw!) that I would go for! If you are interested in learning more about Magnesium supplementation, please ask to speak to our clinically trained Nutritional Therapist Beverley Sarstedt who will be able to advise you and offer suggestions on what is best in your individual case. References: Christina Sun-Edelstein and Alexander Mauskop. “Role of magnesium in the pathogenesis and treatment of migraine.” Expert Review Of Neurotherapeutics Vol. 9 , Iss. 3,2009 E. Wienecke and C. Nolden. “Long-term HRV analysis shows stress reduction by magnesium intake”. MMW Fortschr Med. 2016 Dec;158(Suppl 6):12-16. Epub 2016 Dec 8. |
Amazon Associates DisclosureNourishing Insights is a participant in the Amazon EU Associates Programme, an affiliate advertising programme designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.co.uk. Archives
December 2023
|
WHAT OUR CLIENTS ARE SAYING“I did Nutritional Therapy with Beverley and it was life changing. I highly recommend it!” Allison Blakely (Glasgow)
|
Contact Us |